YourHealthFirst Clinic
AWARD WINNING CLINIC
Health, Dermatology, Hair Loss, Anti-Aging & Rejuvenation Clinic
HARLEY STREET, LONDON est. since 2012
Experts in Rejuvenation without Surgery
Get immediately natural and long lasting results without getting over injected, keeping a natural and most rejuvenated look without over-stuffed look, all treatments are treated with expert hands with many years of experience using the latest techniques and innovations to obtain unbeatable and natural results.
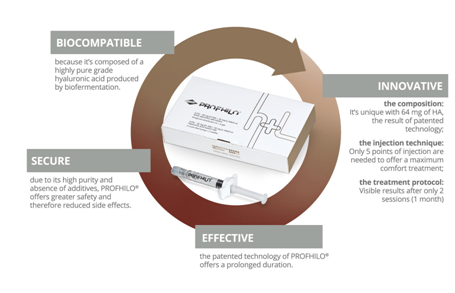
We offer a range of treatments including; Phlebotomy Services (blood draw) Cryolipolysis, Aqualyx and Lemon Bottle both fat dissolving treatment, Botox – Antiwrinkles injections, Dermal Fillers, Eye bags correction, Under eyes dark circles, Rhinomodelation, Revoluminization, Neck rejuvenation, Peeling, Micro-needling, Warts, Skin tags, Moles, Millia & Cherry Angioma removal,Sclerotherapy (spider veins removal), PRP-Platelet Rich Plasma for Hair loss, Hair Thinning, Alopecia Problems, PRP face, neck & hands rejuvenation, Mesotherapy, Profhilo, CryoPen, Acne Scars, Active and Non-active Acne treatment, Rosacea, Stretch Marks, Age Spots, Dark Spots, Melasma, Skin Rejuvenation and more…
Ready to begin your journey?
Book with us to discuss the best options to achieve the results you want, call us today to book a consultation for a customized treatment plan created just for you.
Other Available services; Health Screening – Full body MOT – Visa Medicals & Pre-Employment- Sexual Health Screening – Blood tests –
***Where applicable, certain procedures will be refereed/ carried out by our affiliated clinic, by registered CQC doctor. ***
OUR PROMISE TO YOU
Bespoke Treatments
Everybody is different. We strive to offer treatments that best suit your needs.
We are pioneers in Non-Invasive Aesthetic Treatments
After care
We will do a close follow up after your treatment, to make sure you are happy with the results;
Safety, Aftercare, and Expertise are at the heart of everything we do.
Lasting Results, Natural Process Eliminate Stubborn Fat Cells
Non-invasive procedure for fat reduction.
Permanently and naturally eliminates stubborn fat cells.
No incisions or down-time. You can return to your normal activities immediately.

Our Treatments

anti-wrinkles injections consultation before your treatment if elegible. anti-wrinkles injections are used for the treatment of frown lines, crow’s feet and forehead lines.

Cryolipolysis (Fat Freezing) cryolipolysis lose weight quickly and safely cryolipolysis is the procedure for you if you want to avoid surgery, eliminate stubborn fat, lose weight and return…

sunekos is a new injectable treatment containing amino acids and hyaluronic acid. it works by stimulating the fibroblasts in the skin to produce a complete…
Phlebotomy (blood drawn ) & centrifugal servive yourhealthfirst clinic has been offering private bloods draws and centrifugal since 2014. yhf offers a ‘walk-in’ service,

sclerotherapy involves injecting a solution into blood vessels or lymph vessels that causes them to shrink. it can help with varicose veins or spider veins.

PRP, Face & Body Rejuvenation
non-surgical lift and facial rejuvenation that corrects visual skin defects and promotes the reorganization of its microstructure, all our PRP are injected using the pain…

Mesotherapy meso ox mesotherapy is injected using micro-needling with the pain free, U225 latest intradermal medical injector. Mesotherapy is a non-surgical cosmetic medicine treatment.
Our Photodynamic therapy, is a photosensitive medical peel treatment for rejuvenation and for the treatment of the skin correction…

Vitamin B12 to boost your energy b12 booster shot is popular with many people who want the wide-ranging health benefits that come from having high…

Dermal filler injections are popular fillers and wrinkles treatment options in London. These cosmetic treatments effectively address signs of aging and skin damage by filling in wrinkles, plumping the skin, and targeting deep lines.

Experience the future of aesthetic treatments with pure Exosomes EXO OX at 2 Wimpole St. Our Exosomes treatment is an innovative breakthrough in skin technology and the aesthetic industry, offering the most advanced technology for skin rejuvenation.
Lemon Bottle is the non- surgical fastest and strongest treatment in the industry that targets the Body Fat and reduce it, its quick and convenient with effective results.
NOT SURE EXACTLY WHO WOULD YOU LIKE TO SEE ?
DON’T WORRY !
Our adviser will be sure to book you in the right clinic with the best medical practitioner to meet your needs.
Call Now
T: 0207 225 3582
M : 07818 474 041
Opening hours
Monday to Friday -10am to 6pm
Summer time 10am to 7pm
Saturday -12pm to 4pm - only follow up/or emergency
Sunday -Only by appointment
Out of hours -Only by appointment
Get an appointment